Taking Stock
There’s a joke about travel writers turning experiences abroad into publishable material. Spend two months in China, say, and you can write a book; spend two years, and you can write an article. But spend 20 years, and you find you can’t write anything at all. I feel the same way about the past year of being a medical student. Every day is packed with thousands of stories. Every patient is an epic unto herself. The first few months of being a medical student were an encounter with the world of the hospital. In such a first encounter (with a new book, a new person, a new language), you can ignore the occasional troubling aside and focus on the big picture. But as you get used to things, you can’t avoid the episodes that are harder to talk about.
As a beginning medical student, I was mostly confused. As a fourth-year student who’s just completed his sub-internship (a sort of pre-residency), I’ve become less confused and more intimately involved in the contradictions of the hospital. Once I become a resident, I might become too overwhelmed by life and death to write at all. Now, at the end of this column’s first year, I thought I should take stock of my reactions to what I’ve seen. “Love” and “hate” are the first words that come to mind for many things I’ve encountered this past year. Sometimes I hate and love the same thing in succession.
I hate going into rooms of people who are very sick. They lie in their beds, staring at the wall. What’s the right thing to say to them? Most of the time, as little as possible: I already know this from visiting the sick as a layperson. But as a doctor-in-the-making, I’m no longer someone who visits the sick. I now intrude on them for their own good, asking them questions they would rather not answer and viewing their bodies in ways that they never would countenance when healthy. While I try to build rapport, strengthening the doctor-patient relationship through our basic human connection, more often than not our conversation doesn’t exceed the bare minimum. I need to get my work done; they need to get their rest. So I leave the room feeling guilty, while they lie there feeling no healthier than before.
At the same time, there are patients I come to love even though I know them only slightly. An older, frum woman was admitted with pneumonia. The admitting team described her as demented. According to the technical meaning of the term, this was correct: She suffers from a constant, progressive decline in cognitive function. But too many assume that the demented patient is childlike, not deserving of the respect we would give anyone outside the hospital. I’ve seen more than one demented old woman called “sweetie,” more than one writhing figure in the step-down unit called “nonverbal” while he’s screaming in Yiddish for people to leave him alone. It takes extra effort to listen.
I walked into this woman’s room last Tuesday and asked her how she was. She said something incomprehensible, and I bent closer to hear. “What’s that?” I said, a trifle impatiently. “Ki tov,” she said. “It’s the day of ki tov.” It was Tuesday, the third day, the day that God called good twice. I cried at that — not so anyone would see, of course. I loved that patient even though I didn’t know her at all, because she had said something heartening.
I dislike walking the halls in a long white coat, hearing people call me “Doctor,” running into relatives and families hungry for information that I don’t have or can’t give them. I am the “doctor figure” in whom they find comfort, even though there might be nothing I can do at the moment. At the same time, I try to tell them what I can — even if it’s only the simplest details of the imaging study that’s about to be performed or the tests that are about to be drawn.
There are other reactions that cannot be stopped and break into my best intentions like a freight train. At 5:30 in the evening on the last day of my sub-internship, half an hour before I was due to sign out to the night intern, I was called by a nurse who told me that over the past few hours a patient had become short of breath and incoherent. My first thought, you’ll understand, was not, “Let’s see what we can do to help this poor man.” It was, “Why couldn’t he have waited half an hour?”
But I drew the tests, asked the nurse for an EKG and took the man down for a CAT scan. We tried to figure out what the matter was, piece by piece. Maybe I’ve begun to acquire the everyday discipline that is more important than the drive to do good. Even if it’s half an hour before you’re due to go home, you go do what you’re supposed to. (With your resident, or whoever your boss might be, providing a little push.)
I got into the elevator to go home, and a religious Jewish couple, seeing my yarmulke, gave me a smile. “What a Kiddush HaShem,” they said, using the term for an act or person that shows Jews in a favorable light. I didn’t feel like I had been sanctifying God’s name — I was just learning how to do my job. Do the two overlap? We’ll see.
Zackary Sholem Berger isn’t a doctor yet. Complaints about how long it’s taking should be sent to [email protected].
A message from our Publisher & CEO Rachel Fishman Feddersen

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism during this critical time.
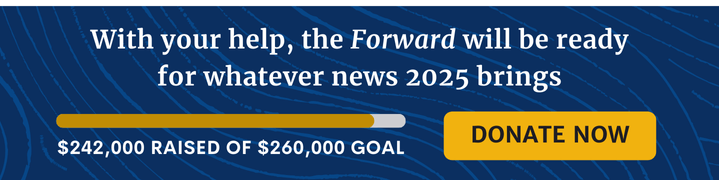
We’ve set a goal to raise $260,000 by December 31. That’s an ambitious goal, but one that will give us the resources we need to invest in the high quality news, opinion, analysis and cultural coverage that isn’t available anywhere else.
If you feel inspired to make an impact, now is the time to give something back. Join us as a member at your most generous level.
— Rachel Fishman Feddersen, Publisher and CEO