Medicine mensch Nau vere bona tratoj So…? How Are Things?
Do you like to talk to other people? Sometimes I do; it depends how many there are. If I’m at a party, I slink toward the chips and-salsa or talk only to my wife. (Wallflowers don’t blossom; they just climb farther up the wall.) If I’m talking to a friend of mine, it can take me some time to shut up. But if I’m face to face with a person who’s providing a paid service — a checkup, a haircut, a repair — I have to remind myself to use the pleasantries that keep ordinary conversation going. I clam up.
Now that I’m almost a doctor, and, more to the point, now that I’m starting a rotation called Ambulatory Care (outpatient medicine, where patients are seen in clinic), I’ll get to see the entire range of patient-conversationalists. But I have to figure out how to talk just enough.
This is both easier and harder than it sounds. Easier because the person you’re talking to gives signals; following those signals is a well-marked route to conversing in a non-annoying fashion. (If the patient is checking her watch, rolling her eyes, or — as in the movie “Airplane” — tying a noose round her own neck, it’s a good sign that her patience is wearing thin.) Talking less is generally good advice in any situation. No one likes a bore, least of all a bore whose favorite topic is your illnesses. Even though patients would like to be fully informed, most of them would like their information in a few concise paragraphs, not in a long-winded discourse.
On the other hand, a doctor needs to talk to get his work done. A silent doctor, like a silent lawyer, invites suspicion. But so does talking: Like lawyer and client, doctor and patient never can have a normal conversation; each of them is waiting for the other word to drop. The patient dreads the openings “There’s something you need to know” or “We need to take a look at that” in the same way that the doctor never can escape the “doorknob questions” that the patient remembers just when she’s about to leave: “Oh, I’ve been meaning to ask you something”; “Just one more thing.”
If the conversation starts off on the right foot, it won’t be so fraught for the parties involved. The accepted pedagogy in medical school is that one must begin in an “open-ended” way, and only later “cone in” to more specific, useful questions. Translated from jargon, this means that ideally the physician would welcome the patient into the office, invite him to sit and then wait silently, like an oracle. If necessary, at the very most one can utter a single word: “Well?” or “So?” Thus encouraged, a patient will spill the whole story without undue interference from the doctor.
If this oracular opening actually were to be adopted in most doctors’ offices, patients would get confused and think they wandered into the psychotherapy suite by mistake. I’ve tried it myself a couple of times, and it spooks the patient. Of course, there’s a compromise available: You can start off without a torrent of detailed questions, but your intro can be friendly and personable.
I’ve tried to see which opener works best for me. There’s “What brings you here today?” An old favorite, but I can never say it without thinking of the old, jokey answer: “A taxi, doctor.” I could ask, “What seems to be the problem?” Fine, I suppose, but it’s nothing I actually would say in the course of a normal conversation. “How are things?” I used that once, and the patient said “Fine, thanks” — and stopped talking right there. I had to restart the conversation from a standstill.
There’s a difference between what’s supposed to happen (according to the theory of the clinic visit) and what actually happens. According to theory, I open up in a general vein and then become more specific as the patient reveals her problems. But the truth is that our conversation only traces the surface of the problems affecting the patient. What people say to their doctors often doesn’t point to the true nature of their ailment. An office visit that the doctor considers notably successful (a problem correctly diagnosed, inroads made into diabetes control or reduction of cardiovascular risk) can appear completely useless to the patient: Her annoying cough hasn’t gone away, and her back still hurts.
This is the conundrum of outpatient medicine. Since the patients seen in hospitals (where young doctors get their start) are sicker on average than they were decades ago, the bulk of today’s training is focused on keeping them alive, or, in rare instances, on curing them. But day-to-day clinic medicine (and the role of doctors throughout much of history) has been not to save lives but to improve them, to make the acute problem less acute and the chronic one easier to bear.
When residents talk, they often say that clinic patients are hard to deal with. Do they mean that hospitalized patients, with their long lists of potentially fatal medical problems, are easy to treat? Maybe it’s that patients in clinic, with their multiple medium-sized problems, come with the same considerable challenges and small-scale opportunities that are present in any interaction. The aim is to make incremental improvements while keeping an eye out for those brief openings that allow a significant change for the good. For the average clinic visit of 10 minutes or so, that’s plenty to talk about.
That’s all we have time for today, I’m afraid. Same time next month?
Zackary Sholem Berger has another patient waiting, but he cares about you personally. Write to him at [email protected].
A message from our Publisher & CEO Rachel Fishman Feddersen

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism during this critical time.
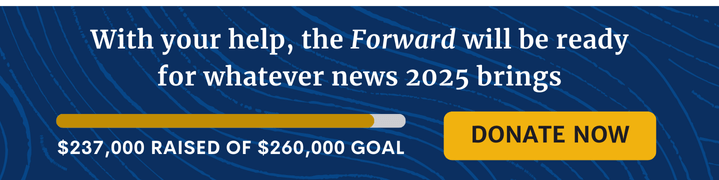
We’ve set a goal to raise $260,000 by December 31. That’s an ambitious goal, but one that will give us the resources we need to invest in the high quality news, opinion, analysis and cultural coverage that isn’t available anywhere else.
If you feel inspired to make an impact, now is the time to give something back. Join us as a member at your most generous level.
— Rachel Fishman Feddersen, Publisher and CEO