The Genetic Mutation That Threatens A Family

Image by Nikki Casey
When Joselin Linder’s father William died of a sudden and debilitating mystery disease in his late 40s, she didn’t realize that it was the marker of a deadly gene that was stalking her family. Twenty years on, she, her sister and her cousins live under the shadow of a gene variant that seems to have uniquely appeared three generations earlier in her family. Although progressing rapidly, genetic science still has no answers for the gene that Linder carries, nor a cure.
I didn’t know Mae. Her eldest child was my grandmother Shirley, whom I knew very well. I called her every day and went to visit her twice a year in Phoenix. When she could, she came to visit me. She told me once that Mae was already the mother of five children the morning her right arm doubled in girth from hand to shoulder.
Shirley was only 12 the day her mother’s arm swelled. When I pressed her about her mother’s illness, she could easily recall the swollen arm, but not what came after. Because Mae probably just wrapped her arm in a cold towel without much fuss, there may not have been much to remember.
Mae’s swollen arm, unbeknownst to anyone, signaled the beginning of a harrowing, if slow-moving, fight for her life as her health mysteriously began to deteriorate. Her doctors did what little they could to ease her earliest symptoms. Her swollen arm was a nuisance and a physical disfigurement, but it wasn’t life-threatening. One doctor sent her home with a manual pump she’d wrap around her arm, using air pressure from the pump like a massage to keep the fluid loose.
Mae, married to my great-grandfather Rabbi Morris (Pittsfield’s first Orthodox rabbi) used it for many years before she went to bed at night.
Meanwhile, Mae’s other tests continued to come back normal. But when, three years later, her breathing became labored due to fluid leaking into her lungs — much like in my father’s case — all bets were off. Mae was 38 years old. Her children ranged in age from 4 to 14. Not being able to breathe wasn’t an option. At the hospital, doctors were able to “tap” her, draining off some of the fluid that had settled into her chest, taking some of the pressure off her lungs.

Image by Aaron Fanin
The first time Mae was tapped, she watched as an alarmed and confused medical team extracted about 50 milliliters of lemon-meringue-yellow fluid from her chest. No one knew where it had come from, but Mae’s doctors charged forward with a few ideas about what might be causing her labored breathing.
Officially, Mae had been diagnosed with pleurisy, a condition in which a series of membranes covering the lungs, called “pleura,” become inflamed. It is a symptom of tuberculosis (TB), which in the 1930s often proved fatal. By 1938, doctors at Mount Sinai Hospital in New York had tested Mae’s fluid for bacteria and ruled out TB. What they knew was that her lungs were filling with fluid, and they had to do something to drain it off.
To treat her, the doctors decided to follow the same protocol they used for other breathing disorders of the day: Mae would sleep outside and live in relative seclusion.
Two years after she woke up with a swollen arm, Mae and her husband took their oldest child, 14-year-old Shirley, for a walk, leaving the other kids at home. They told Shirley that her mother was going to go away for a while to a hospital to help her breathe.
Mae was sent to Coolidge Memorial Hospital on the southwest side of Pittsfield, twenty miles from the family’s home. Patients with tuberculosis, contagious and otherwise, lived in tents about half a mile downhill from the main building, where Mae took up sleeping quarters on a beautiful wraparound screened-in porch with three to four other patients, all TB patients undergoing treatment.
When Mae was released from Coolidge Memorial, after six months, her condition had stabilized. She began visiting Mount Sinai Hospital in New York City, undergoing exploratory procedures to seek out the cause of the fluid that was steadily, if slowly, increasing. She stayed for weeks at a time with her parents in Brooklyn, a four-hour journey by train from the Berkshires. On several occasions she brought Yussy, her youngest child. Mostly, though, Yussy was left with his grandmother or one of his sisters.
Ten years after the appearance of her first symptoms, when her oldest children were married with children of their own, Mae began undergoing radiation treatments in a “we’ll try everything even if we don’t know what we’re treating” sort of spirit. Radiation treatments were the conventional recommendation for many life-threatening illnesses. In order to receive the treatment, Mae walked to Pittsfield General Hospital, often with Rabbi Morris, Shirley, or Norma, who helped out on her visits home from New Jersey. After the treatments, Mae usually threw up in the street — a side effect of the radiation.
By 1955, nearly 20 years after Mae woke up to that swollen right arm, the accumulation of fluid in her body had become unbearable. She underwent repeated tapping procedures to extract as much of it as possible, but by midsummer, the tissue around her lungs had become so scarred that the fluid was unreachable. Shirley, by now a mother of three and living with her in-laws, helped out when she could. When her father instructed her to accompany her mother to see yet another specialist, this time across the state in Boston, she reluctantly agreed, feeling as she did that it was her father’s responsibility to accompany his wife to the appointment. But Shirley was not the only family member whom Mae’s protracted illness was making into a martyr.

Decisions about Mae’s treatment were left to a reluctant Shirley. A doctor at the Pratt Diagnostic Center wanted to put her broken body through a deeply invasive procedure called a “thoracotomy.” He told Mae and Shirley that her chance for survival was 50-50. A thoracotomy involves a chest and abdominal incision that opens up the skin, muscle, and rib cage in order to gain access to the patient’s heart and lungs. Cutting open skin riddled with lymph is always dangerous. Even a small, everyday cut can easily become infected, so larger, more prominent incisions risk deadly infections. In a woman whose body was already in a weakened state, it’s likely Mae’s chances were far worse than 50-50. But the Pratt doctor was the only one with a plan. And Mae couldn’t breathe, so she couldn’t afford to be choosy.
Shirley gave the okay for the operation, which was performed at Albany Hospital on August 22, 1955. Her father joined her in the hospital waiting room during the five-hour procedure. Immediately following the surgery, the incision the doctor had made began to fester. Over the next two weeks, Mae’s condition remained touch and go. Finally, on September 9, 1955, she died. The infected thoracotomy scar on the left side of her chest noted in the report was listed as the primary cause of death — although the gross quantities of lymph fluid in every region of her body were cited as a contributing factor. She was 55 years old.
Over 17 years, Mae endured debilitating bouts of breathlessness and exhaustion, not to mention painful and disfiguring swelling. But she did continue to live for those seventeen years. She got to meet eight of her 12 grandchildren. There is no shortage of black-and-white photographs showing her lovingly holding Billy, her oldest grandchild. She was able to watch him grow into a little boy. But she never once imagined that the flaws in her own body would become the tragic legacy that would bind them together.
Joselin Linder is a writer living in Brooklyn. She regularly contributes to the New York Post, and has contributed to NPR’s This American Life and Morning Edition, among other outlets. Follow her on Twitter, @joselinder
Excerpted from “The Family Gene: A Mission To Turn My Deadly Inheritance Into A Hopeful Future.” Copyright © 2017, published by Ecco.
A message from our Publisher & CEO Rachel Fishman Feddersen

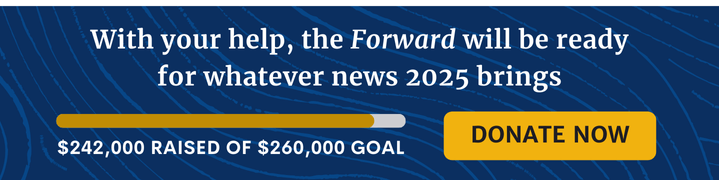
I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism during this critical time.
We’ve set a goal to raise $260,000 by December 31. That’s an ambitious goal, but one that will give us the resources we need to invest in the high quality news, opinion, analysis and cultural coverage that isn’t available anywhere else.
If you feel inspired to make an impact, now is the time to give something back. Join us as a member at your most generous level.
— Rachel Fishman Feddersen, Publisher and CEO