Was She at Risk for Cancer or Wasn’t She?

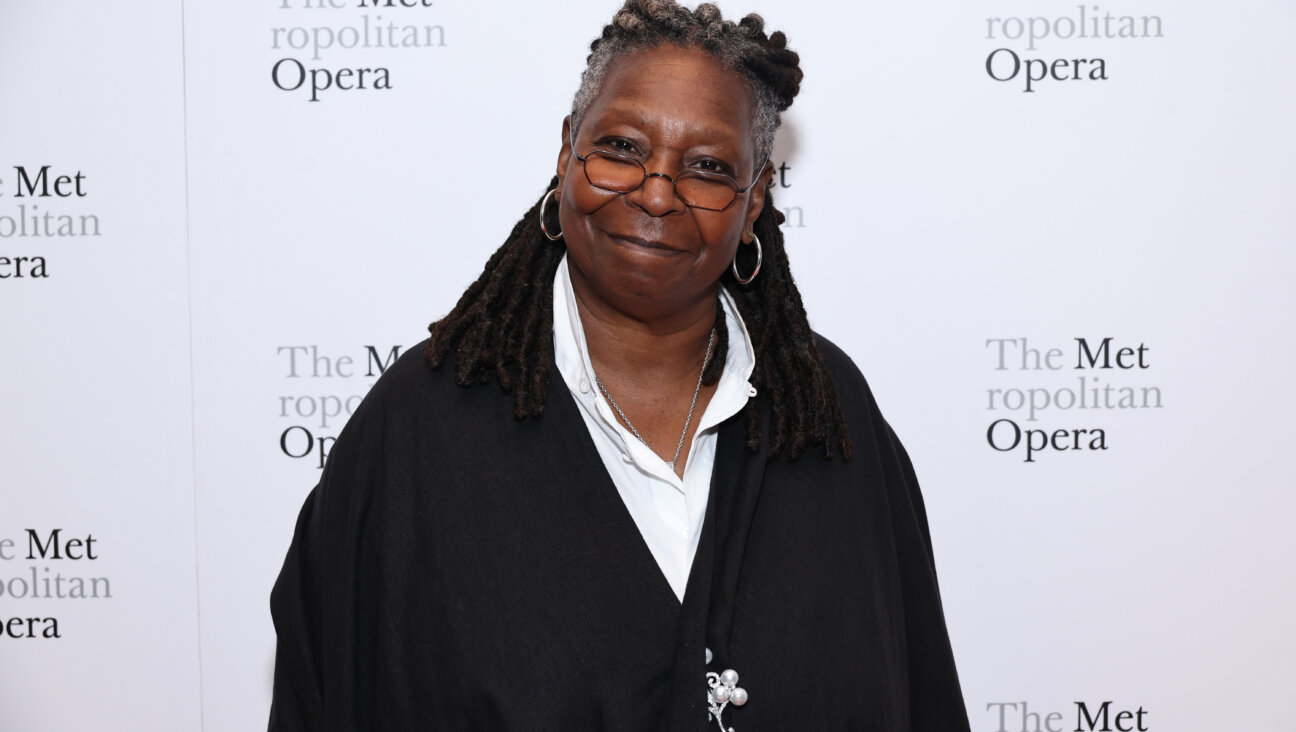
Generations of Unknown Risk: Dorothy Brown, the author (far left), her mother and her grandmother, holding Brown’s newborn daughter. Image by courtesy of dorothy brown
As a newlywed in the 1970s, I watched my vibrant, stylish maternal grandmother go from trim to gaunt. She and my grandfather had raced their family out of Vienna the day Hitler marched in. But now she was diagnosed with an ovarian tumor the size of an orange, too late for treatment to save her life. She died a year later, at age 74. I was overwhelmingly sad, but as a 29-year-old, I didn’t see the implications for me. The genetic links to breast and ovarian cancer had yet to be discovered. Families could only wonder and worry.
Little did I realize that over the next 40 years I would come to a decision on a question troubling many others like me: How much risk for a deadly disease had I inherited and what should I do when science has yet to offer answers?
The next shoe dropped in 1992. My mother, now approaching the age of my grandmother and fearing she would die the same way, insisted on a CT scan. It revealed an irregularity on an ovary. After major surgery, she announced that it had been a “pre-cancer.” No follow-up was needed. She was fine.
I continued with life, raising three daughters, blissfully ignorant of any health risk to myself. But that changed in 1994, when scientists announced a link between the BRCA mutations and breast and ovarian cancer. Over the next decade, as more research emerged, I became increasingly concerned — not just for myself, but also for my girls.
About 1 in 40 Ashkenazi Jews is a carrier of a BRCA mutation, compared with 1 in 500 in the general population. Had my grandmother and my mother, who had died at age 75 of an apparently unrelated brain tumor, been afflicted by these genes gone awry? Even scarier for our daughters: my husband’s mother and her sister had both died of breast cancer in their 50s. If our parents and their siblings carried the BRCA mutations, there was no way of knowing: They were all gone.
I began wondering what the pathology of my mother’s ovaries had really shown. She sometimes spun the truth to make herself look better, telling dinner guests, for instance, that she’d made the elaborate dessert when, in fact, she had bought it. What was this “pre-cancer” she had had? My ob-gyn had no idea what that meant. Had my mother invented that phrase to justify her fears and major surgery?
A sympathetic archivist at Columbia Presbyterian Hospital dug up long-buried records. They stated that my mother had had a tumor of “low malignant potential.” What did that mean? The tissue slides, which might have offered a definitive answer, had not been kept.
With genetic testing now readily available, my husband and I decided to get screened. Great news! Neither of us carried any of the major BRCA culprits! We cheered and happily announced to our daughters that they were free of that worry, anyway. We also urged our siblings to get tested. Perhaps we were the lucky ones in the roll of the genetic dice.
As for myself, I pretty much stopped worrying. Ovarian cancer is relatively uncommon, affecting about 1.4% of women over the course of their lives.
Three years later, in 2007, lightning struck: My husband’s sister Janice, age 53, was diagnosed with ovarian cancer. She had been vigilant about getting regularly checked for breast cancer — which had killed her mother and aunt — but she had not heeded our advice to go for genetic tests. They would have revealed that she had inherited a BRCA1 mutation, perhaps in time to take action. The risk of ovarian cancer for women with BRCA1 is upwards of 40% by age 70, according to the National Cancer Institute. About 65% will develop breast cancer.
The next 3 1/2 years were gut wrenching as our brave and beautiful Janice switched from one chemo cocktail to the next. Each eventually failed. At Janice’s bedside, days before her death, her son and the woman he would marry pledged their love to each other. Her daughter’s new boyfriend and future husband — who would never know his mother-in-law — stood at Stefanie’s side through the funeral and shiva.
I vowed I would never endure that death or impose that suffering on my children. Within weeks, I had met with Dr. Thomas C. Randall, a gynecological surgeon then at the University of Pennsylvania (now at Massachusetts General Hospital), to discuss my grandmother’s cancer, my mother’s odd pathology, and my own risk, even with no known BRCA mutation. I might face only the 1.4% risk of the general population, he said. Or, because of my family history, my risk could be higher, if some unknown genetic variant was lurking. He reminded me that 80 to 90% of ovarian cancer is not associated with BRCA. And of that 80 to 90%, we still don’t know how much could be explained by a yet-to-be-determined familial cause, and how much is caused by a spontaneous mutation.
If I decided to have my ovaries removed, I faced the risk of surgical complications and the loss of whatever lingering protection estrogen, produced in the ovaries, had for my heart and bones as a post-menopausal woman. (The issue is particularly significant for younger women.) Regular ultrasounds of my ovaries, on the other hand, were unlikely to catch anything in time. “There may be no such thing as Stage 1 in some types of ovarian cancer,” Dr. Randall warned. The decision was up to me.
I left his office unsure. A few months later, as I grieved for Janice and dawdled over my decision, a friend called. She was having bloating and stomach pains — the vague, often overlooked symptoms that can characterize ovarian cancer. I leapt at the news. Something in me, perhaps my Holocaust survivor’s heritage, intuitively knew it was time to run. That afternoon I scheduled surgery and didn’t cancel when my friend’s symptoms proved a false alarm. My ovaries were removed through laparoscopic surgery, with three tiny incisions. I went home that afternoon and have had no apparent ill effects.
Since then, as someone concerned about the uninsured and the climbing cost of medicine, I’ve wondered whether I took advantage of my good health insurance to selfish ends. Was all this unnecessary?
Dr. Mary B. Daly, chair of clinical genetics at the Fox Chase Cancer Center in Philadelphia and chairperson of the National Comprehensive Cancer Network’s panel on breast and ovarian cancer risk, recently reassured me and confirmed Dr. Randall’s view.
In my case, it was “not terribly unreasonable to have oophorectomy,” Dr. Daly said. “Based on the fact that it looks like a genetic risk and we haven’t found a test and there’s no screening, it may come down to a personal choice — one [that] insurance should pay for,” she added. “You could argue that if you got ovarian cancer it would cost a lot more. And you can’t measure the value of your own peace of mind.”
Not that the worrying ever ends. Dr. Daly thought it might be wise for me to get screened with the newer genetic tests. Down the road, my daughters may want to know.
Dorothy Brown is former medical and science editor for the Philadelphia Inquirer. She blogs at www.unRetiring.blogspot.com.
A message from our Publisher & CEO Rachel Fishman Feddersen

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism so that we can be prepared for whatever news 2025 brings.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
Readers like you make it all possible. Support our work by becoming a Forward Member and connect with our journalism and your community.
— Rachel Fishman Feddersen, Publisher and CEO