Non-Jews Hit by ‘Jewish’ Diseases Fall Through the Cracks of Genetic Screening

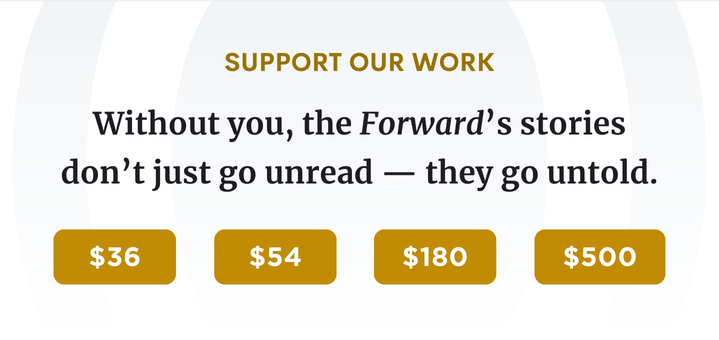
Family History: Randy Yudenfriend-Glaser, the chair of the Jewish Genetic Disease Consortium (second from left), and her husband, Jordan, in a family portrait, hold children Jonathan and Lauren who have ML4, a genetic metabolic disease. Image by Courtesy of Randy Yudenfriend-Glaser
For three days in April, about 70 families whose lives have been upended by Tay-Sachs disease gathered in San Diego for the annual National Tay-Sachs and Allied Diseases conference. The event — which attracted families caring for children with Tay-Sachs, as well as those who have lost loved ones to the degenerative disease that claims most of its victims by age 4 — included forums on symptom management and new research frontiers. There were also support group sessions and a candle-lighting ceremony honoring those who had died.
Tay-Sachs is probably the best known “Jewish” disease. As many as one in 25 Ashkenazi Jews is a carrier of the defective recessive gene. Yet, among the conference attendees, who came from as far away as Poland and Guatemala, only a handful were Jewish. “When I speak with newly diagnosed families, they often say, ‘But we’re not Jewish,’” said Kimberly Kubilus, NTSAD’s director of family services.
Today, the vast majority of babies born with the disease are not Jewish. Of the approximately 15 new infantile Tay-Sachs cases diagnosed in the U.S. each year “maybe one is from a Jewish family,” Kubilus said. The disease leads to paralysis, blindness, seizures and eventually total incapacitation and death.
At a recent conference on Canavan disease — for which one in 40 Ashkenazi Jews is a carrier — Canavan Foundation President Orren Alperstein met just one family that reported Jewish ancestry. The other 15 or so families she encountered were not Jewish. “I was surprised by [the demographic makeup], but more surprised that there were several families there who had more than one child with Canavan,” said Alperstein, whose 7-year-old daughter, Morgan, died of the disease in 1997.
Canavan, which is generally diagnosed in infancy, results in severe mental retardation and paralysis. The average life span of a child born with the disease is three to 10 years, though there have been rare cases of those surviving into their 20s. Like Tay-Sachs and other illnesses under the “Jewish genetic disease” umbrella, it is an autosomal recessive disease, which means that two carrier parents have a one in four chance of having an affected child.
With carrier screening widespread in the Jewish community, some genetic diseases such as Tay-Sachs have been “all but screened out of the Jewish population,” said Randy Yudenfriend Glaser, the mother of two children with mucolipidosis IV who chairs the Jewish Genetic Disease Consortium. Testing has dramatically reduced the overall number of children born with these illnesses, as Jewish carrier couples increasingly use assisted reproductive technology to become pregnant with a healthy child or elect to terminate an affected pregnancy.
By contrast, non-Jewish couples are not likely to have been recommended for the same battery of tests. Even in the rare case that they are screened for Jewish-linked diseases, the standard DNA test is highly effective in picking up only the most common mutations, those found in the Ashkenazi Jewish population. (On the other hand, enzyme tests, which measure the amount of specific enzymes in the blood, are better able to identify the rarer mutations found outside a disease’s home ethnic groups.)

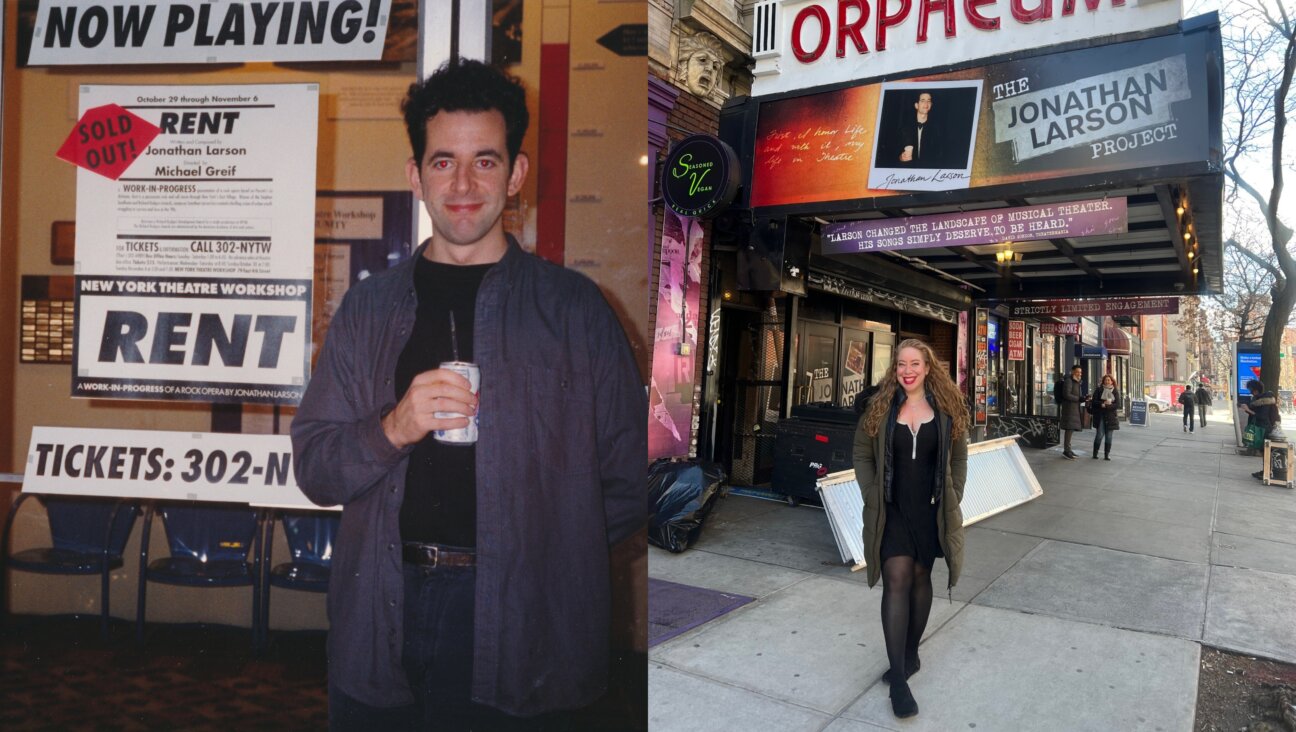
Emily Rapp with her son, Ronan, who died of Tay-Sachs disease in February. Image by Soulumination.org
Awareness and availability of screening for Jewish genetic diseases “has been great for Ashkenazi Jews, but not so great for non-Jewish people, and there are a lot of us,” said Emily Rapp, whose 2-year-old son, Ronan, died of Tay-Sachs in February. Rapp, who in March published “The Still Point of the Turning World” (Penguin Press), a memoir about parenting a critically ill child, was given the DNA test, not the enzyme test, when she requested prenatal screening for Tay-Sachs. She is not Jewish, but her husband is.
Genetic screening for Tay-Sachs has been available for more than three decades. Yet there are still widespread misconceptions among health care providers, rabbis and the general population about who is at risk for Jewish genetic diseases, who should undergo carrier screening and how those tests should be done, JGDC’s Yudenfriend Glaser said. “I can’t tell you how many people say, ‘Oh, I’m married to a non-Jew’ or ‘Oh, I’m going to get married to a non-Jew. I don’t need to worry about that,’” she said. “Is it a smaller likelihood? Yes, but we’ve seen enough Tay-Sachs babies” to know that interfaith couples are still at risk.
Also at risk are couples in which neither partner is Jewish. Although mutations for certain genetic diseases may be far more common in Ashkenazi Jews and some other high-risk populations, they can also be found in the general population. One in every 300 people is thought to be a carrier for Tay-Sachs; one in every 200 for Gaucher. But for many other Jewish diseases, the general carrier frequency is unknown because screening for these mutations has focused on high-risk populations. In addition to Ashkenazi Jews, high-risk ethnic groups include French-Canadians, Irish and Cajuns for Tay-Sachs, Afrikaners for Fanconi anemia Type C and Pennsylvania’s Mennonites for maple syrup urine disease, according to JGDC.
When Tim Lord’s son, Hayden, was one year old, he was diagnosed with cerebral palsy. Six months later, as his motor skills continued to regress, Hayden was re-evaluated and found to have Tay-Sachs — a diagnosis the doctor had originally ruled out because neither of his parents is Jewish. “We were working with one of the top pediatric neurologists in Manhattan, and it never occurred to him that a non-Jewish couple could have a child with Tay-Sachs,”
‘We’ve seen enough Tay-Sachs babies to know that interfaith couples are still at risk.’said Lord, whose son died in 2000 at age 2.The daughter of Lord’s identical twin died of the same disease the following year. Lord says he understands why carrier-screening efforts have centered on populations known to be at high risk. But he said he’d like the scientific community to “move toward a more universal testing environment, using the power of computers and the power of gene sequencing.”
Some scientists are critical of the practice of linking genetic diseases with ethnic identity. In the American Journal of Public Health, Sherry Brandt-Rauf of the University of Illinois, Sheila Rothman of Columbia University and other researchers said such linkages “exaggerate genetic differences among ethnic groups” and may result in “health disparities” in groups not targeted for screening.
A more level testing field may not be that far off. The medical genomics firm Counsyl, for example, offers screening for up to 100 diseases for $99 for clients with insurance plans. Those without accepted health coverage pay $599. “I think it makes sense to move away from an ethnicity-focused approach to carrier screening, particularly now that testing is more affordable,” said Shivani Nazareth, a genetic counselor with Counsyl.
She noted that the panel of prenatal DNA tests that are standard for Ashkenazi Jews already include diseases, such as spinal muscular atrophy, that are not necessarily more common in the Jewish population. “If the point is to give families better options for reproductive planning,” Nazareth said, “and there is affordable carrier screening for additional disorders … then why limit access based on ethnicity?”
Gabrielle Birkner is a Forward contributing editor and co-founder of the forthcoming website ModernLoss.com. Follow her on Twitter @gabibirkner
A message from our Publisher & CEO Rachel Fishman Feddersen

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism so that we can be prepared for whatever news 2025 brings.
At a time when other newsrooms are closing or cutting back, the Forward has removed its paywall and invested additional resources to report on the ground from Israel and around the U.S. on the impact of the war, rising antisemitism and polarized discourse.
Readers like you make it all possible. Support our work by becoming a Forward Member and connect with our journalism and your community.
— Rachel Fishman Feddersen, Publisher and CEO