Experts: Testing for Breast and Ovarian Cancers Still Lags
When Wendy Mailman’s mother, Eloyce, was diagnosed with ovarian cancer last February, her concerned daughter immediately began scouring the Internet for information.
Through medical sites and an ovarian cancer listserv, Mailman learned that women of Eastern European Jewish descent were at an increased risk for inheriting a predisposition for both breast and ovarian cancer. One out of 40 individuals of Ashkenazic Jewish descent is at risk. That risk, Mailman found, could be detected through testing for two genetic mutations, the so-called BRCA 1 and BRCA 2.
Looking back, Mailman is shocked that her mother’s gynecologic oncologist did not introduce the option for genetic testing or even inquire about her mother’s ethnic background.
“She was treated in the suburbs of Philadelphia, where there is a decent-size Jewish community,” said Mailman, who is also a medical professional, an anesthesiologist.
“He just didn’t ask the questions,” Mailman said of her mother’s doctor. “I mentioned it to him after a very long conversation about my mother’s initial treatment. ‘We’re Jewish,’ I said. ‘Should my mom get testing?’ And he said, ‘Yeah, she should get tested,’ but I am convinced he would never have brought it up.”
Such scenarios are very common, Adi Bar-Lev said. As a genetic counselor, Bar-Lev has seen people fall through the cracks for both testing and the counseling step that should precede it. Even if a doctor orders the testing, Bar-Lev said, if he or she fails to refer the patient for counseling, “the patient is really losing an opportunity to learn more for themselves about what their options are.”
Bar-Lev and her colleagues are the conduits through which patients receive essential information about their family history and associated health risks before deciding whether to be tested. Counselors advise patients of what can be learned from a genetic test and what that test’s limitations are.
People testing positive for a BRCA mutation, for example, will not necessarily develop cancer in their lifetime. But the test can’t tell them this — only that they are at a much greater risk than the general population. Disseminating such facts to worried patients and their families is critical — but it doesn’t always take place.
Prompted by her daughter’s research, Eloyce Mailman tested for the BRCA mutations and learned she was negative. That information was crucial not only for knowing if her daughter and other family members were at risk for ovarian cancer, but also because women with ovarian cancer are themselves more likely to develop breast cancer. If Eloyce had tested positive, she could have used that knowledge, perhaps electing to have preventive care such as a prophylactic mastectomy.
That procedure is well known to the public as a preventive treatment for those with a family history of breast cancer, but it is only one of several components now available for women who are at risk for the disease, said Noah Kauff, a cancer geneticist at Memorial Sloan-Kettering Cancer Center in New York.
“For example, one of the most important developments in screening women with inherited risk is the addition of breast MRI to mammography,” Kauff said, adding that the procedure substantially improves the ability to detect early breast cancer in women who have an inherited risk.
Researchers have not yet found a definitive screening tool for ovarian cancer; a transvaginal ultrasound in conjunction with a blood test has been used, with mixed results. Medical experts, however, have isolated symptoms of the disease: bloating; pelvic or abdominal pain; difficulty eating or feeling full quickly, and urinary symptoms.
Kauff said that other pieces of information on ovarian cancer can be discovered via genetic testing. “Our screening for ovarian cancer is not optimal, but we have also learned a great deal about the timing of the risks,” he said. For example, for women with the BRCA 2 mutation, the majority of risk of ovarian cancer occurs after menopause. “Only 2 to 3 percent of women with the BRCA 2 mutation develop ovarian cancer before they are 50,” he said.
In the past decade, Kauff said, the genetics community has experienced significant advancement.
“We now have good evidence that we can alter the natural history of inherited predisposition,” he said. “We can make it not only less likely that women with these predispositions will die of cancer, but even less likely that they will get cancer at all.”
A message from our Publisher & CEO Rachel Fishman Feddersen

I hope you appreciated this article. Before you go, I’d like to ask you to please support the Forward’s award-winning, nonprofit journalism during this critical time.
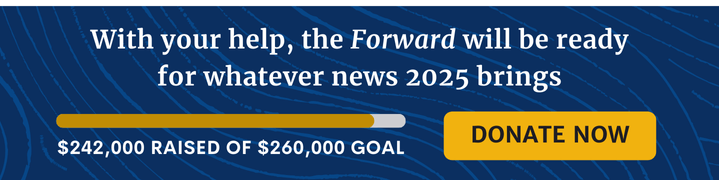
We’ve set a goal to raise $260,000 by December 31. That’s an ambitious goal, but one that will give us the resources we need to invest in the high quality news, opinion, analysis and cultural coverage that isn’t available anywhere else.
If you feel inspired to make an impact, now is the time to give something back. Join us as a member at your most generous level.
— Rachel Fishman Feddersen, Publisher and CEO